Some treatment options are available, but the condition is progressive and incurable. Although it is not a widely known disease, even non-sufferers will find certain facts about TN interesting and unsettling.
10 A Long History
Discussions about facial torture (tortura oris) can be traced back to the ancient Greek physicians Galen and Aretaeus of Cappadocia in the first century and Avicenna in the 11th century. Even Hippocrates found versions of this facial pain a notable mystery in his writings. The next reports of the condition appear in Somerset, England, in the 13th century. At the tomb of Bishop Button, one can see wall carvings of people depicted as suffering severe facial agony. Historians suggest that this was a reference to what we now know as trigeminal neuralgia and not just toothaches. Button’s skeleton was later exhumed, and it possessed a set of nearly perfect teeth. Nevertheless, Button had been canonized and travelers came to give offerings at his grave in the hopes that the saint would relieve their toothaches. Trigeminal neuralgia hit the mainstream medical world when famous physician John Locke described it in 1677. It received its first medical term, tic douloureux, from Nicolas Andre in 1756. Shortly after Andre’s study, John Fothergill wrote the first comprehensive description and understanding of the condition, and it was dubbed “Fothergill’s disease.”[1] Fothergill identified it as a neurological condition rather than pains caused by the teeth, mouth, or tongue. Modern neurology now classifies it as trigeminal neuralgia, a reference to neuropathy of the fifth cranial nerve (the trigeminal nerve).
9 A Disease Of Many Names
One can’t deny the shock value of trigeminal neuralgia’s most famous and chilling colloquial name—the “suicide disease.” Many sufferers are dismayed to learn the term when they are newly diagnosed, although they are likely to relate to the gravity and seriousness of it. Trigeminal neuralgia produces excruciating pain for the sufferer and is known as the worst pain a person can experience. Effective treatments have only recently been discovered.[2] With no way to escape the world’s most unimaginable pain, more than 50 percent of sufferers were believed to have committed suicide. However, sufferers (and their loved ones) will be comforted to know that there is no substantial evidence or statistic to support this claim. Less worrisome monikers for trigeminal neuralgia include tic douloureux, Fothergill’s disease, prosoplasia, and trifacial neuralgia. The most common term used by sufferers and those who treat trigeminal neuralgia is simply “TN.”
8 Trigger-Happy Pain
So what triggers the facial spasms and electric-like bolts in a TN sufferer’s face? A better question might be: What doesn’t? Those who suffer from this condition report a wide array of triggers. Commonly reported culprits include smiling, touching your face, brushing your teeth, brushing your hair, wind, eating and drinking, changes in temperature, shaving, putting on makeup, certain foods, loud noises, and kissing. The list goes on, and sufferers often report that just the fear of triggering an episode can cause them to withdraw from their daily activities.[3]
7 The Dental Connection
“Yank ’em all out!” This is likely the battle cry of most new TN sufferers before proper diagnosis. Like the shrine of Bishop Button, TN patients look like people who are suffering from dreadful toothaches. Their first course of action is to see a dentist to remove the offending teeth, not knowing that it is actually facial nerve pain as it radiates to the nerve endings in the jaw. Many TN patients unnecessarily have teeth removed. They think that it’s the cause of their pain, and dentists can acquiesce to their demands if they aren’t familiar with the condition or given a proper diagnosis. This can be a sad, frustrating process for both patient and doctor as they learn that the pain persists despite the onward march to a full set of dentures before age 50. Unfortunately, this is a common warning tale among veteran TNers when counseling new patients.[4] The dental connection is not totally misguided, however, as research has shown that dental problems can often be the cause (rather than the effect) of TN facial pain. Accidental or iatrogenic dental trauma is found to be the cause of nearly 40 percent of all cases of trigeminal neuralgia. When combined with trigger-inducing standard dental work and the ongoing perception of tooth pain, this can give new meaning to having a “dental phobia.”
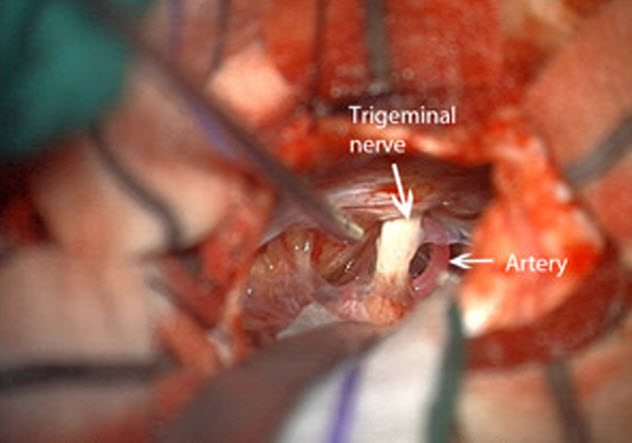
6 Treating The Incurable
Given the long history of trigeminal neuralgia, it is surprising that viable treatment options for the condition have only been discovered within the last century. Once the disorder was linked to neurological origins, doctors were able to more effectively develop medical interventions. Since it is a nerve condition, traditional painkillers like NSAIDs and opioids do not touch the pain. Anticonvulsant and seizure medications like gabapentin and Trileptal are the first line of defense. They work in about 80 percent of the cases. However, patients report difficult side effects and often have to increase their doses over time to maintain the efficacy of the drugs. Other pharmaceutical options include Lamictal and Baclofen to augment the effects of the anticonvulsants. When the medication doesn’t work on its own (and it often doesn’t), TN patients have a number of surgical options. The most common is microvascular decompression (MVD) surgery. This procedure was developed by Walter Dandy in 1925 and has quickly come to be the most popular of the TN surgical options.[5] MVD is a brain surgery that involves separating the root of the trigeminal nerve from a compressing artery that is aggravating the nerve. This procedure is often quite successful for patients with Type 1 TN whose MRI images show that compression is the main culprit. Long-term results of MVD are varied, with some patients reporting full relief but only for a limited time. This can mean multiple surgeries and the risk of debilitating surgical side effects such as anesthesia dolorosa. For those patients with Type 2 TN or another condition called atypical face pain, MVD may not be the prescribed intervention. Other surgical options exist, such as rhizotomy, glycerol injections, and balloon compressions. So where do all these options leave us? At the same place we started. TN is an enigmatic and fierce foe to the neurological sciences. Some treatments work—but only for some and only for so long. Managing a treatment plan for TN is a full-time job. It takes a lot of trial and error, perseverance, and commitment from both doctor and patient. The research is happening. So with some good luck (and a few good scientists), a cure or at least a long-term, reliable treatment may be just around the corner.
5 Triple Whammy
Trigeminal neuralgia is known to coexist with a few other dastardly houseguests. As if the feeling of your face being pierced by ice picks and electrocuted by lightning while your teeth feel weighted down by 10-ton dumbbells isn’t enough, now you’ve got to throw in the extra perks of a down-and-out trigeminal nerve. The most commonly known comorbidity with TN is multiple sclerosis.[6] Scientists have yet to determine the nature of the connection or which comes first—the proverbial chicken or the egg. (However, it is noteworthy that 1–2 percent of MS patients have TN as their first symptom.) Researchers have identified a chilling rate: 18 percent of women with TN also have a diagnosis of MS, and 2 percent of all MS patients have TN. To make it even worse, 5 percent of all TN–MS patients suffer from bilateral facial pain, a rare type of TN as it usually only makes its home on one side of the face. Another problem for TN sufferers is migraines and cluster headaches. These three tend to travel in groups, although one is not thought to cause the others. Some doctors theorize that this may be due to the proximity between migraines and cluster headaches with the trigeminal nerve itself, resulting in an interconnected web of aggravation, pain, and secondary symptoms. It is also important to note that a common side effect of TN medications is headache. Sometimes, the TN anticonvulsant therapies can help prevent migraines and other headaches, but many times, the migraines and headaches must be treated with their own therapies and interventions. It wouldn’t be far-fetched to assume that a person’s mental health and well-being would be gravely affected by the ravages of this condition. Depression is a frequent companion of TN patients, and their doctors and caregivers should give attention to and support for this unfortunate outcome. A person’s life changes drastically when they get trigeminal neuralgia. This includes fear during the process of diagnosis (not knowing what’s happening to them), adjusting to life with chronic pain, loss of ability to do things they normally enjoyed, and an overall loss of hope. Support groups (online and in person) are available to help with the adjustment and in finding understanding and sympathy for their changing life conditions.
4 Differential Diagnosis
The right diagnosis at the right time can make all the difference in a person’s ability to understand, treat, and cope with trigeminal neuralgia. To avoid the long, frustrating road of misdiagnosis, experts recommend these steps. First, if you have tooth pain, see a dentist. Ask if he is familiar with trigeminal neuralgia. If he is, encourage a differential diagnosis before getting any teeth extracted. If he isn’t, leave. Second, make an appointment with a neurologist as soon as possible. These are the folks who understand the condition and how to help you. It may take some time to see one in your area, but you can work on a temporary plan with your primary care physician in the meantime. Third, if you have to go to the emergency room due to the severity of the pain, be prepared to have your pain questioned. ER docs aren’t TN specialists, so offer what you know about the condition. (Have it on a piece of paper because you’ll likely be in too much pain to talk.) Also ask if they have a neurological consultant on hand. Remember, typical painkillers and opiates will only help the pain mildly. The first form of emergency intervention is a fosphenytoin IV (otherwise known as Dilantin). Ask the doctors about it. (Again, having the information on hand will really help you out when you’re in extreme pain.) After you get a full workup from your neurologist, you can ask him to write an emergency care plan to bring to the ER with you to avoid any questions or confusion about what you need. Finally, you may be able to diagnose yourself. A leading international researcher and neurologist on trigeminal neuralgia has created a self-diagnosis tool. He believes that it can guide anyone through a reasonably accurate diagnosis of face pain.[7] It is available here. Once you’ve come up with your likely diagnosis, take it with you to doctor appointments. With any luck, it will help the diagnosis journey go more smoothly and you will feel empowered.
3 Famous Faces
Trigeminal neuralgia is indeed rare, but it has still affected some current celebrities and historical figures. Social activist and writer Gloria Steinem has spoken out about her challenges with trigeminal neuralgia. Steinem describes the condition as excruciating. When it flares, it renders her speechless and unable to walk. HR, the singer of famed rasta band Bad Brains, underwent his own “bad brain” surgery to deal with his TN. Using GoFundMe, HR and his family raised $16,000 for the surgery and have reported that he is doing well now.[8] In 2011, Bollywood actor Salman Khan announced that he had trigeminal neuralgia and had flown to the United States to receive treatment. Khan used his position as a celebrity to spread awareness about the disease. He stated, “If there was a choice to give this pain to my worst enemy, I would not give it. They wouldn’t be able to take it.” In 2015, Member of Parliament Andrea Jenkyns was chided by the media for being unable to finish the words in a public speech. Jenkyns spoke out against the reports by citing trigeminal neuralgia as the cause of her difficulty. She described the disorder as “excruciating” and “sporadic.”
2 Gaining Recognition
The facial pain and TN societies have fought long and hard for advanced research into and increased awareness of trigeminal neuralgia. On October 5, 2017, the United States House of Representatives passed House Resolution 558 which recognizes October 7 as National Trigeminal Neuralgia Awareness Day. It also expresses the government’s commitment and support toward finding an end to the disease. The facial pain network is also seeking international recognition of October 7 as International Trigeminal Neuralgia Awareness Day through the World Health Organization. This proposal was submitted on July 1, 2017.[9] Additionally, TN is gradually gaining more coverage in various news stories, TV shows, and short films. As the condition is put in the spotlight, sufferers will learn that they are not alone, researchers and scientists will be encouraged to search for a cure, those who live or work with TN sufferers will gain a greater understanding of the disorder, and the medical community will become more generally aware of the condition to reduce future misdiagnoses.
1 The Good (Forget The Bad And The Ugly)
It’s hard to believe that there is any good news after all the unsettling facts discussed above. But there is. If you suffer from TN or know someone who does, there are many resources and “best practices” you can follow to make the journey a bit more bearable and hopeful. Check these out . . . experts say they are well worth it. Connection: Get involved in the Facial Pain Association,[10] TNnME, and social media support groups. Self-Care: Now more than ever, you have to be your No. 1. Know your triggers, and have a plan for dealing with them. Make a plan with your family as to how you will work as a group to deal with episodes. Find ways to relax and self-soothe, and commit to them. Pain Management: Consider seeing a doctor who specializes in pain management. These specialists have alternative approaches to managing and coping with pain that many TN patients have found quite helpful. Be Your Own Advocate: Know your condition from top to bottom—your exact diagnoses, your test results, your medications, your ER visits, and your doctors. Keep a file of all relevant medical information, and take it with you to all doctor and ER visits. Be the master of your medical records, and advocate for yourself! Sometimes, Michael likes to write.